The Role of Virus-Specific T Cells in Modern Immunotherapy
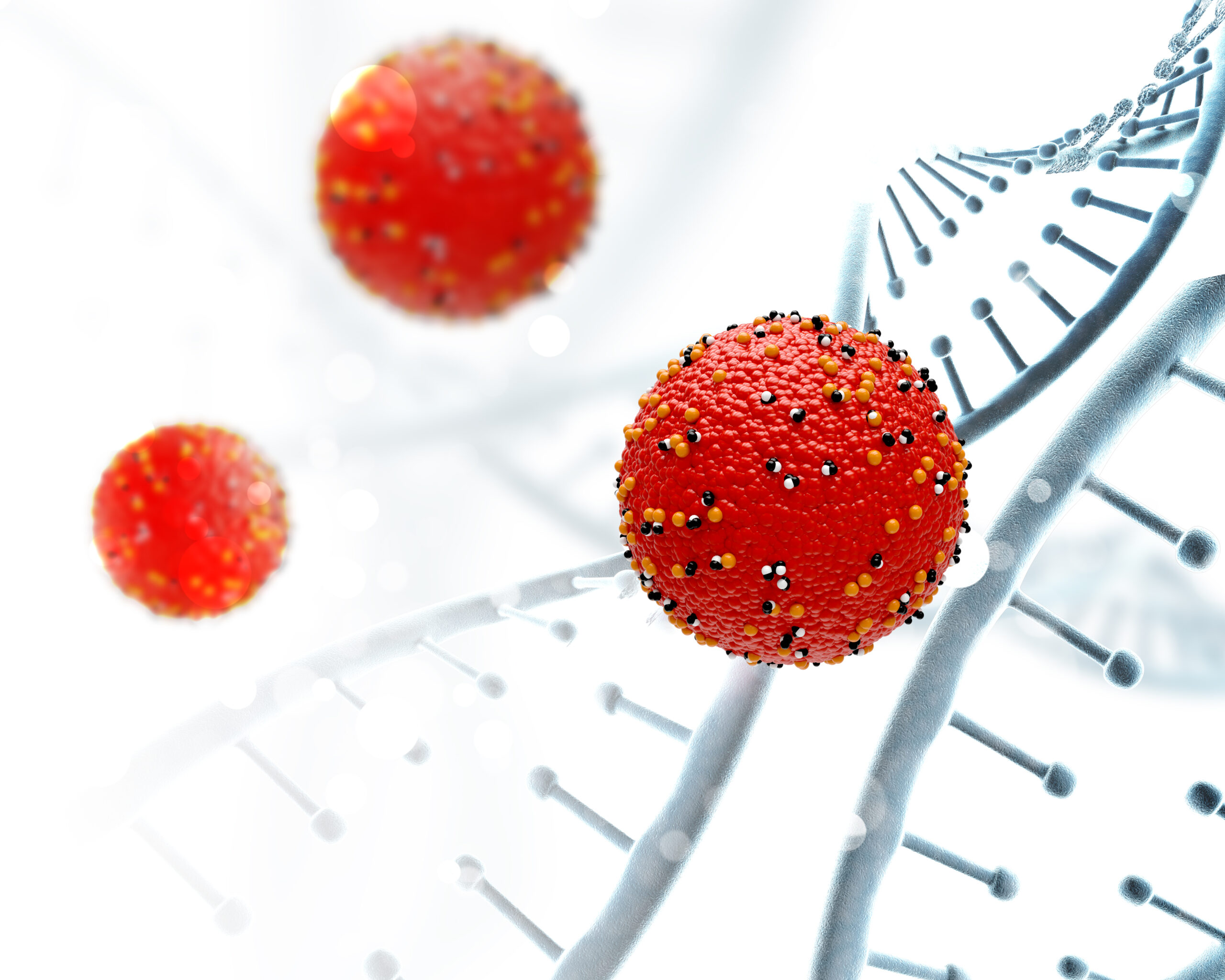
Immunotherapy has revolutionized the way we approach infectious diseases and cancer, harnessing the body’s own immune system to target specific threats. Among the most promising strategies in this field is the use of virus-specific T cells (VSTs). These specialized immune cells have the unique ability to recognize and eliminate virus-infected cells with high precision, offering targeted, potent, and personalized therapeutic options. In this article, we explore the role of virus-specific T cells in modern immunotherapy, their clinical applications, and how organizations like Xellera Therapeutics are advancing the field.
Understanding Virus-Specific T Cells
T cells are a crucial component of the adaptive immune system, capable of identifying and destroying infected or malignant cells. Among them, virus-specific T cells are a subset programmed to recognize viral antigens presented on infected cells. Once activated, these cells can proliferate rapidly and mount a focused immune response, eliminating infected cells while sparing healthy tissue.
Unlike broad-spectrum antiviral drugs, VSTs offer specificity and durability. By targeting only the virus-infected cells, they minimize collateral damage to the patient’s healthy cells, reducing side effects often seen in conventional therapies.
Applications in Infectious Diseases
One of the most well-established applications of virus-specific T cells is in treating viral infections in immunocompromised patients, such as those who have undergone bone marrow or stem cell transplantation. Common viral pathogens in these populations include cytomegalovirus (CMV), Epstein-Barr virus (EBV), and adenovirus. Conventional antiviral therapies may be insufficient due to resistance, toxicity, or delayed immune recovery.
VST therapy provides a powerful alternative by restoring pathogen-specific immunity directly. Several clinical studies have demonstrated that infusion of VSTs can reduce viral load, control persistent infections, and improve patient survival rates, making it an indispensable tool in post-transplant care.
Cancer Immunotherapy
Beyond infectious diseases, virus-specific T cells also play a growing role in oncology. Certain cancers, particularly those associated with viral infections like EBV-positive lymphomas or HPV-related cancers, can be targeted using VSTs. By recognizing viral antigens expressed on tumor cells, these T cells selectively attack malignant cells without harming normal tissues.
The specificity and adaptability of VSTs make them an attractive option for personalized cancer immunotherapy. Researchers are exploring ways to engineer T cells to recognize tumor-associated viral antigens more efficiently, combining immunotherapy with other modalities such as checkpoint inhibitors and CAR-T therapies.
Advantages of VST Therapy
Virus-specific T cell therapy offers several key advantages over conventional treatments:
Precision: VSTs target only virus-infected or virus-associated tumor cells.
Durability: These cells can persist in the body, providing long-term immunity.
Reduced toxicity: Unlike antiviral drugs or chemotherapy, VSTs minimize damage to healthy tissues.
Personalization: T cells can be expanded or engineered to match the patient’s viral profile, enhancing efficacy.
These benefits underscore why VSTs are considered a promising frontier in both infectious disease management and cancer treatment.
Manufacturing and Quality Considerations
Producing virus-specific T cells for clinical use requires specialized facilities, expertise, and strict adherence to Good Manufacturing Practices (GMP). The process involves isolating T cells from the patient or donor, stimulating them with viral antigens, expanding them to therapeutic numbers, and ensuring safety and potency before infusion.
Organizations like Xellera Therapeutics are at the forefront of enabling GMP-compliant VST manufacturing. By providing state-of-the-art infrastructure, advanced quality control systems, and regulatory expertise, Xellera Therapeutics helps translate cutting-edge research into safe and effective therapies that meet rigorous clinical and regulatory standards.
Challenges and Future Directions
Despite their potential, VST therapies face several challenges. Generating sufficient cell numbers, ensuring long-term persistence, and overcoming immune evasion by viruses or tumors remain active areas of research. Additionally, broadening the accessibility of VST therapies to more patients worldwide requires scalable manufacturing processes and streamlined regulatory pathways.
Emerging innovations, such as off-the-shelf allogeneic VST products and gene-edited T cells, aim to address these challenges. With ongoing research and technological advancements, virus-specific T cells are poised to become a mainstay in both infectious disease and cancer immunotherapy.
Conclusion
Virus-specific T cells represent a powerful and precise approach to modern immunotherapy. Their ability to selectively target virus-infected or virus-associated cells offers significant advantages in terms of safety, efficacy, and personalization. As clinical research progresses and manufacturing capabilities expand, VST therapies are expected to play an increasingly prominent role in treating viral infections and virus-related cancers.
With the support of specialized CDMOs like Xellera Therapeutics, researchers and clinicians can leverage advanced GMP-compliant production and quality systems to bring these innovative therapies to patients safely and efficiently. By combining scientific expertise, technological innovation, and regulatory excellence, VST therapies are shaping the future of targeted immunotherapy worldwide.